How Neurorehabilitation Helps With Stroke Recovery


Victims of a stroke, especially those with substantial brain damage, may see both their lives and those of their families change drastically post stroke. The sufferer has to adapt to life without certain capabilities and settle into a different way of living than what they were used to, which has social consequences.
However, improvements in brain activity through neurorehabilitation in occupational therapy, physical therapy, and the like, have proven promising in recovering these abilities. With successful neurorehabilitation, patients have hope to reclaim both their movement and their previous quality of life.
What is Neurorehabilitation?
Neurorehabilitation utilizes the help of occupational therapy and physical therapy with patients and their families to build back the skills and attitudes of people affected by hemiparetic stroke. The main goal is to get their skills to work at the highest level, so patients can rebuild self-esteem and a positive mood. Recovering from a stroke can be a long, almost hopeless process, but with the new adaption skills patients learn, they become empowered and gain the skills for community reintegration.
Neurorehabilitation therapies teach or retrain patients how to improve or recover their communication and mobility skills, as well as other aspects of their daily lives. In its treatments, neurorehabilitation focuses on the psychological, creative, and nutritional elements of each individual’s recovery.
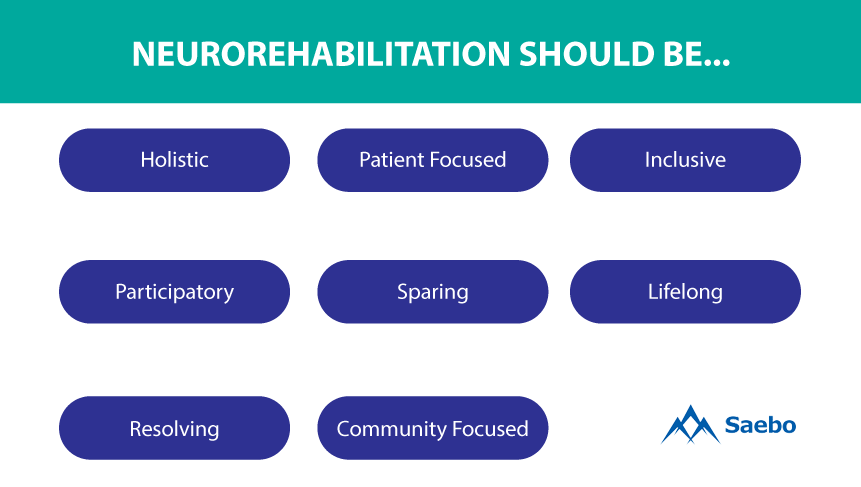
- Holistic. Provide not only physical and cognitive recovery, but also include psychological, social, and cultural aspects of the patient's personality and those of their family.
- Patient focused. Health-care strategies customized to the needs of the patient and their family.
- Inclusive. Developed and implemented by multidisciplinary teams of qualified and motivated practitioners experienced in similar types of collaboration.
- Participatory. Patient and family are actively involved and build a trusting relationship, work together with the team of medical professionals.
- Sparing. Help the patient maximize independence and reduce physical impairment, dependence on mobility aids.
- Lifelong. Supports and follow-up carried out from injury onset to the highest possible level of recovery of function, even later in life.
- Resolving. Include adequate resources for efficiently attending to each patient's difficulties as they arise.
- Community focused. Find solutions that best fit aspects of the community and create resources that assist the patient in social reintegration.
Customized Neurorehabilitation
Neurorehabilitation can be divided into measures that aim to (1) help the patient adapt to or compensate for their impairments or (2) reduce impairments. The latter addresses underlying neurological deficits more directly but is relatively poorly understood.
Various neurorehabilitation programs, which are offered by hospitals or at private, specialized clinics, have a broad range of professionals in different neurophysiologic areas to provide the most comprehensive treatment and customized approach to allow patients and their families to live more normal lives.
Each year, newer methods and neurophysiologic technologies are developed and implemented, allowing more opportunities for patients. Since the field of neurorehabilitation is relatively new, however, many strategies are controversial because they don’t yet have the research to support their results.
Neuroplasticity and Rehabilitation
Neuroplasticity is the adaptation and ability of the brain and rest of the central nervous system (CNS) to change and adapt in response to cues. In doing so, it encodes these cues as experiences and learns new behaviors. For many years, mainstream neuroscience contended that brain plasticity was limited to early childhood. But it has since been discovered that the brain is continuously in the plasticity stage. Today, it is known that significant brain remodeling can be induced at any age in life and that a damaged brain also has this ability to recover lost skills and behaviors.
Neuroplastic processes include changes at molecular, biochemical, synaptic, dendritic, axonal, morphological, and connectomic levels. Considering this, therapy strives to enhance and activate plastic changes in the therapeutic window after a stroke.
Neurorehabilitation and Movement
One of the most promising tracks in neurorehabilitation is movement. In learning again how to move a part of the body affected by stroke, for example, the brain’s plasticity changes. Activity takes advantage of neuroplastic changes and enhances them to help with stroke recovery. Decreases, increases, recruitment of additional brain regions, and shifts in brain activation can help facilitate behavioral improvement during occupational and physical therapy.
Learning skills is more important for functional reorganization than simply repeating movements. Practice is vital to this process, but it must be varied and spaced out for patients to be able to retain and generalize these skills. For example, a therapist can direct a patient to reach out and hold onto a glass the same way at the same distance during each practice session, or they can instead change the distances and speeds at which the patient reaches for the object. Varied practice will allow patients to add to their skills long term and better adapt to daily living.

A patient’s progress depends in large part on their doses of therapy—in other words, the hours of practice they put in. Usually the more the practice, the better the outcome. For instance, logging thousands of motor repetitions and at least 100 hours of language practice leads to the best results. Some ways to encourage more practice are by assigning home video hand/arm training, robotic arm and treadmill training, and eye search and reading therapies.
Helpful Motor Learning Exercises (Recruitment and Retraining)
The following are methods that use motor learning to enable patients to successfully rehabilitate and relearn how to move to carry out their needs successfully. They can be used in combination or practiced in stages as patients progress.
Arm ability training. Aimed at patients with mild hemiparesis that have clumsiness and weakened coordination even though they may have normal neurological examinations. These patients are the most likely to return to work after their stroke. The arm ability training tasks include hand grip, finger individuation, arm-hand steadiness, aimed reaching, tracking, and wrist-finger speed.

Constraint-induced movement therapy (CIMT). This movement technique has two parts and is usually carried out over two weeks. The first part is restraint of the non-affected extremity for 90 percent of waking hours. The second part is an intensive practice with the affected extremity for six hours a day using shaping. In patients with chronic hemiparesis, the restraint can help patients overcome learned non-use, whereas in patients with an acute stroke it can be seen as a way to prevent the adoption of compensatory strategies with the unaffected limb.
Electromyogram (EMG)-triggered neuromuscular stimulation. It uses sensorimotor integration theory, which says that non-damaged motor areas can be recruited and trained to perform more efficient movements using time-locked, movement-related afference. The Saebo MyoTrac Infiniti can help with the needed EMG-triggered neuromuscular stimulation involved in initiating a voluntary contraction for a particular movement until the muscle activity achieves a threshold level. When EMG activity reaches the determined threshold, the assistive electrical stimulus is triggered. In this, two motor learning principles can be joined in one order: repetition and sensorimotor integration.

Interactive robotic therapy. This movement method is congruent with the sensorimotor integration theory in EMG-triggered neuromuscular stimulation. Patients begin a movement, are assisted in completing it via a robot-assisted device, and so are reinforced in a command leading to movement.
Virtual reality-based rehabilitation. Patients can have a virtual teacher or a video game help them properly perform daily living arm movements in real time. Therapies like the Saebo ReJoyce and others can help keep patients engaged and get the repetitions needed for learning and rebuilding.
Behavioral Compensation and Neuroplasticity
Another problem that can come up during movement therapy is behavioral compensation. Behavioral compensation is the brain’s response to damage and behavioral attempts to make up for that impairment. When the reaction to behavioral experiences improves functional reorganization and outcomes, the brain achieves functional recovery.
The key to fuller recovery lies in patients relearning how to move properly so they are able to realize their needs.
While the brain builds new pathways and renews former ones during therapy, different body parts compete for representation in the brain. Both the ipsilateral and contralateral hemispheres play a part in motor control: if one hemisphere is harmed, the other may adopt some of its functions. So, it is vital to promote sensory stimulation in the forms of electrical signals, massaging, neuromuscular facilitation exercises, and generally stimulating senses to aid recovery.
To achieve the greatest benefits, physical movements should focus on specific tasks and be repetitive. For instance, it is important for the patient to retrain themselves to perform functional tasks such as rolling in bed, sitting, standing up, and walking.
Key Points of Successful Rehabilitation
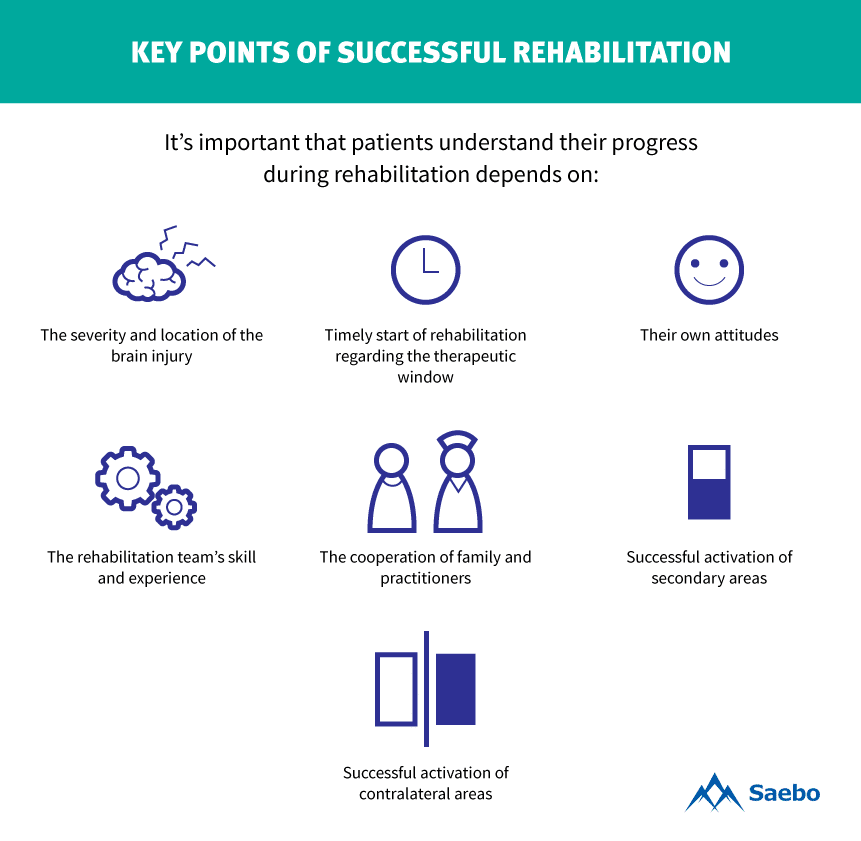
It’s important that patients understand their progress during rehabilitation depends on:
- Timely start of rehabilitation regarding the therapeutic window
- The severity and location of the brain injury
- Their own attitudes (daily commitment to exercise)
- The rehabilitation team’s skill and experience
- The cooperation of family and practitioners
- Successful activation of secondary areas
- Successful activation of contralateral areas
Getting Back to Normal Life
Stroke neurorehabilitation is a progressive and dynamic process aimed at enabling patients to reach their optimal physical, cognitive, emotional, communicative, and social functional levels.
This method of therapy offers a number of exercises to help patients recover lost motor functions and reduce damage caused by a stroke. Neurorehabilitation also provides lifelong support needed by patients and their families as they rejoin a community. It allows motivated patients to reach their ultimate goals of reclaiming independence and returning to normal life.
All content provided on this blog is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, call your doctor or 911 immediately. Reliance on any information provided by the Saebo website is solely at your own risk.
All content provided on this blog is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. If you think you may have a medical emergency, call your doctor or 911 immediately. Reliance on any information provided by the Saebo website is solely at your own risk.



